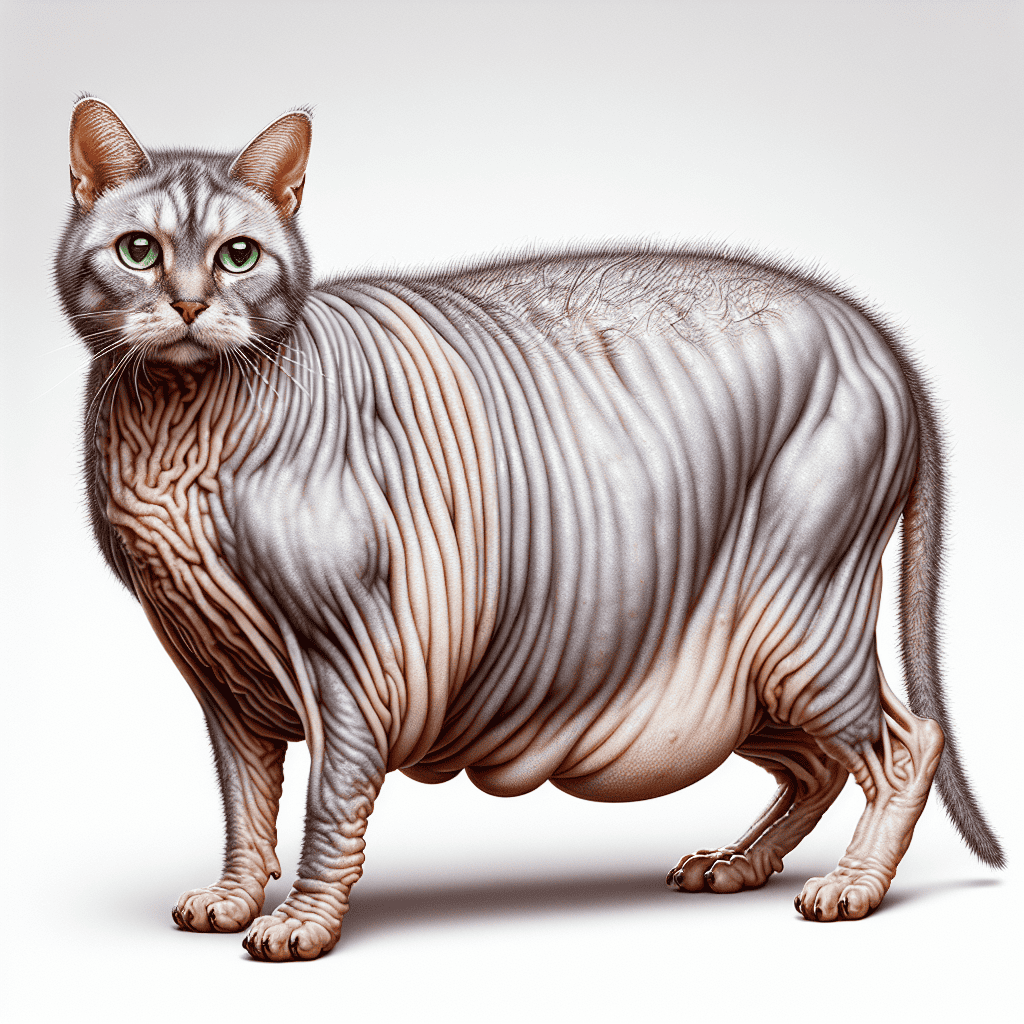
Understanding Cushing’s Disease in Cats
Cushing’s disease, also known as hyperadrenocorticism, is a relatively uncommon condition in cats. It occurs when there is persistent excessive production of the hormone cortisol from the adrenal glands, which can be caused by abnormalities of the pituitary gland or the adrenal glands themselves (International Cat Care). While hyperadrenocorticism is more common in dogs, it can still occur in cats, and successful treatment is possible.
What is Cushing’s Disease?
Cushing’s disease in cats is characterized by the overproduction of cortisol, a hormone that plays a vital role in various bodily functions. Excessive cortisol concentrations can lead to several abnormalities in cats, including:
- Excessive thirst (excessive thirst in cats)
- Weakness
- Skin changes (hair loss in cats)
- Slow-healing wounds
- Diabetes mellitus
- Increased appetite (increased appetite in cats)
Causes of Cushing’s Disease
There are different causes of Cushing’s disease in cats, including:
-
Naturally-occurring hyperadrenocorticism: This form of the disease is primarily caused by adrenal or pituitary tumors. Adrenal-dependent disease accounts for less than 15% of naturally-occurring hyperadrenocorticism, with some cases involving underlying malignant tumors like adrenal carcinoma. Pituitary-dependent disease is more common and is often due to small benign tumors called microadenomas (International Cat Care).
-
Iatrogenic hyperadrenocorticism: This type of hyperadrenocorticism is induced by the long-term administration of high doses of cortisol-like drugs. These drugs can include corticosteroids or progesterone-type drugs, which are sometimes used to control reproductive cycling in female cats.
Understanding the underlying cause of Cushing’s disease is crucial for determining the most appropriate treatment approach. Diagnostic tests, such as blood tests and imaging studies, are typically performed to identify the cause and confirm the diagnosis of Cushing’s disease in cats.
By understanding what Cushing’s disease is and its potential causes, cat owners can recognize the signs and seek proper veterinary care. Early detection and appropriate treatment can help manage the condition and enhance the quality of life for cats affected by hyperadrenocorticism.
Symptoms and Diagnosis
Identifying the presence of hyperadrenocorticism, commonly known as Cushing’s disease, in cats can be challenging due to its varied symptoms. However, recognizing these symptoms and obtaining a proper diagnosis is crucial for effective treatment. In this section, we will explore the common symptoms exhibited by cats with Cushing’s disease and the diagnostic tests used for its identification.
Common Symptoms in Cats
Cats with hyperadrenocorticism may display a range of symptoms, although they can vary from cat to cat. Some of the most frequently observed symptoms include:
- Excessive drinking and urination: Cats with Cushing’s disease may exhibit increased thirst (excessive thirst in cats) and increased urination. These symptoms are often indicative of the body’s attempt to eliminate excess cortisol.
- Increased appetite: Affected cats may experience an insatiable appetite (increased appetite in cats) and may exhibit weight gain as a result.
- Lethargy and weakness: Cats with Cushing’s disease may appear lethargic and weak due to the impact of elevated cortisol levels on their energy levels.
- Muscle wasting: The disease can lead to muscle wasting, causing a decrease in muscle mass and overall muscle strength.
- Hair loss: Cats may experience hair loss (hair loss in cats) or thinning of the fur, particularly along the back and sides.
- Thin and fragile skin: The skin of cats with Cushing’s disease may become thin and fragile, making it prone to bruising and injury.
It’s important to note that these symptoms can also be indicative of other health conditions. Therefore, it is crucial to consult with a veterinarian for a proper diagnosis.
Diagnostic Tests for Cushing’s Disease
To confirm the presence of hyperadrenocorticism in cats, veterinarians utilize a combination of diagnostic tests. These tests help evaluate cortisol levels and identify the underlying cause of the disease. Common diagnostic tests for Cushing’s disease in cats include:
- Baseline lab work: Blood tests are performed to assess various parameters, including liver and kidney function, blood cell counts, and hormone levels. These tests provide a baseline for comparison during further diagnostic evaluation.
- Urine cortisol measurements: Urine samples may be collected to measure cortisol levels. Elevated cortisol in the urine can indicate hyperadrenocorticism.
- ACTH-stimulation test: This test involves administering a synthetic hormone called ACTH to stimulate the adrenal glands. Blood samples are collected before and after the administration to measure cortisol levels. Abnormal cortisol responses can help diagnose Cushing’s disease.
- Dexamethasone suppression test: In this test, dexamethasone, a synthetic glucocorticoid, is administered to assess the body’s cortisol response. Elevated cortisol levels after administration can indicate Cushing’s disease.
In some cases, additional diagnostic imaging tests such as x-rays or ultrasounds may be performed to evaluate the adrenal glands and identify any tumors or abnormalities.
By recognizing the common symptoms associated with Cushing’s disease and utilizing appropriate diagnostic tests, veterinarians can accurately diagnose hyperadrenocorticism in cats. Timely diagnosis is essential to initiate appropriate treatment and enhance the cat’s quality of life.
Treatment Options
When it comes to treating Cushing’s disease (hyperadrenocorticism) in cats, there are several options available depending on the underlying cause and severity of the condition. The two main treatment approaches for Cushing’s disease in cats are medical management and surgical interventions.
Medical Management
Medical management is often the first line of treatment for Cushing’s disease in cats. The primary medication used for medical management is trilostane. Trilostane has shown significant improvement in clinical signs and adrenal function in cats with hyperadrenocorticism, with studies reporting positive outcomes in approximately 87% of cases (NCBI). It is considered the safest and most effective treatment option for cats with pituitary-dependent hyperadrenocorticism (NCBI).
Trilostane works by inhibiting the production of cortisol, the hormone that is overproduced in Cushing’s disease. By regulating cortisol levels, trilostane helps alleviate the symptoms associated with the condition, such as hair loss, excessive thirst, and increased appetite.
It is important to note that medical management requires lifelong treatment and close monitoring to ensure the medication’s effectiveness and adjust the dosage as needed. Regular check-ups and follow-up blood tests are necessary to evaluate treatment response and maintain the cat’s well-being.
Surgical Interventions
In certain cases of Cushing’s disease, particularly those associated with adrenal tumors, surgical intervention may be necessary. Surgical treatment options include removing the tumor(s) through adrenalectomy or, in cases of pituitary-dependent hyperadrenocorticism, hypophysectomy (removal of the pituitary gland).
Adrenalectomy involves the removal of the affected adrenal gland(s) responsible for excessive cortisol production. This surgery aims to eliminate the source of the hormone overproduction and alleviate the associated symptoms. However, not all cats with Cushing’s disease are suitable candidates for surgery, and the decision to proceed with surgical intervention depends on factors such as the cat’s overall health and the location and size of the tumor.
Hypophysectomy is a specialized surgical procedure that involves removing the pituitary gland. This surgery is primarily performed in cases of pituitary-dependent hyperadrenocorticism. While hypophysectomy can be an effective treatment option, it is a complex procedure that requires highly skilled veterinary specialists.
Both surgical interventions carry some risks and require careful consideration by the veterinarian and the cat’s owner. Post-operative care and regular follow-up visits are essential to monitor the cat’s progress and ensure a successful recovery.
The choice between medical management and surgical interventions depends on various factors, including the type of Cushing’s disease and the individual cat’s overall health. A thorough evaluation by a veterinarian, including diagnostic tests, will help determine the most appropriate treatment approach for managing Cushing’s disease in cats.
Prognosis and Quality of Life
When it comes to Cushing’s Disease in cats, the prognosis and quality of life can vary depending on various factors such as the cat’s overall health, response to treatment, and the underlying cause of the disease. Let’s explore the prognosis for cats with Cushing’s Disease and the considerations for their quality of life.
Prognosis for Cats with Cushing’s Disease
The prognosis for cats with Cushing’s Disease can be positive, especially for those that receive appropriate treatment. Cats who respond well to treatment and have the offending steroid removed can experience an improved quality of life. However, it’s important to note that individual responses to treatment can vary.
The treatment of Cushing’s Disease in cats may involve a controlled gradual withdrawal of steroids, alternative medications, medications like Trilostane to suppress cortisol production, surgery (adrenalectomy or hypophysectomy), or radiation depending on the underlying cause of the disease (PetMD). Regular monitoring and follow-up visits with a veterinarian are crucial to assess the cat’s response to treatment and adjust the treatment plan if necessary.
It’s important to keep in mind that while treatment can improve the cat’s condition, Cushing’s Disease is a chronic condition that requires ongoing management. With proper care and treatment, most cats with Cushing’s Disease can experience an improved quality of life.
Quality of Life Considerations
Maintaining a good quality of life for cats with Cushing’s Disease involves several considerations. Managing the clinical signs associated with the disease, such as excessive thirst (excessive thirst in cats), increased appetite (increased appetite in cats), hair loss (hair loss in cats), and muscle wasting, is crucial to ensure the cat’s comfort and well-being.
In addition to medical management, providing a suitable environment for the cat is essential. This includes creating a stress-free and comfortable living space, ensuring a balanced diet and proper hydration, and offering regular exercise and mental stimulation. Regular veterinary check-ups and follow-up visits are also important to monitor the cat’s condition and make any necessary adjustments to the treatment plan.
It’s essential for cat owners to work closely with their veterinarians to ensure that their cats receive the appropriate care, treatment, and support needed to maintain a good quality of life. By following the recommended treatment protocols and providing a nurturing environment, cat owners can help their furry friends live happy and fulfilling lives despite their diagnosis of Cushing’s Disease.
In the next section, we will delve into the differentiation between pituitary and adrenal tumors in Cushing’s Disease and the various treatment approaches for each.
Pituitary vs. Adrenal Tumors
When it comes to hyperadrenocorticism, or Cushing’s disease, in cats, it is important to differentiate between pituitary and adrenal tumors. Understanding the differentiating factors and treatment approaches for each type can help guide the management of this condition in cats.
Differentiating Factors
Cushing’s disease in cats can be caused by three different factors: pituitary gland tumor, adrenal gland tumor, or iatrogenic Cushing’s disease from prolonged use of steroids. Pituitary gland tumors are the most common cause, accounting for approximately 80%-85% of cases. Adrenal gland tumors and iatrogenic Cushing’s disease make up the remaining cases.
Differentiating between pituitary and adrenal tumors is crucial for determining the appropriate treatment approach. In cases of pituitary-dependent hyperadrenocorticism, the tumor is located in the pituitary gland, which is responsible for regulating hormone production. Adrenal tumors, on the other hand, originate from the adrenal glands, which are located near the kidneys and produce hormones involved in stress response.
Treatment Approaches
The treatment approaches for pituitary-dependent hyperadrenocorticism in cats may involve medical management, radiation therapy, or surgical treatment.
-
Medical Management: Trilostane is a medication commonly used for the medical management of pituitary-dependent hyperadrenocorticism in cats. According to a study, trilostane improved clinical signs and ACTH stimulation test results in 87% of cats with hyperadrenocorticism (NCBI). However, it is worth noting that trilostane may not cause remission in some cats, especially in cases with pituitary enlargement, as it can worsen neurological signs (NCBI).
-
Radiation Therapy: Radiation therapy (RT) is another treatment option for cats with pituitary tumors. The goal of RT is to decrease the size of the tumor and ameliorate clinical signs and insulin resistance. However, it is important to note that RT has been reported to be only partially successful in treating hyperadrenocorticism with pituitary tumors. The RT protocol can vary, with some studies using a single 15-Gy dose or multiple doses of 15-20 Gy (NCBI). The response to RT can vary among individual cats, with some showing improvement in clinical signs while others may experience adverse effects or require euthanasia due to other diseases (NCBI).
-
Surgical Intervention: Surgical treatment, known as hypophysectomy, involves the removal of the pituitary gland tumor. This procedure is complex and not commonly performed due to the delicate nature of the pituitary gland and associated risks. Surgical intervention is typically considered a last resort when other treatment options have been exhausted.
The choice of treatment approach for hyperadrenocorticism in cats depends on various factors, including the individual cat’s overall health, the extent of the disease, and the availability of specialized veterinary care. It is important to work closely with a veterinarian to determine the most appropriate treatment plan for each cat.
By understanding the differentiating factors and treatment approaches for pituitary and adrenal tumors in cats with hyperadrenocorticism, veterinarians and cat owners can make informed decisions regarding the management of this condition. Regular monitoring and follow-up visits with a veterinarian are essential to assess the response to treatment and make any necessary adjustments to ensure the best possible outcome for the cat’s health.
Case Studies and Research
To gain a deeper understanding of hyperadrenocorticism in cats and its management, let’s explore some successful management cases and the latest research findings.
Successful Management Cases
One notable case study involved a 10-year-old castrated male cat diagnosed with hyperadrenocorticism and pituitary macroadenoma, along with insulin-dependent diabetes mellitus. The cat underwent radiation therapy as part of the treatment plan. The radiation therapy involved a linear accelerator delivering 4 Gy per fraction, totaling 48 Gy over 12 fractions. After radiation therapy, a significant decrease in pituitary tumor size (10.7 mm) was observed on day 301, along with remission of neurological and dermatological signs (NCBI). This case study highlights the potential effectiveness of radiation therapy in managing hyperadrenocorticism in cats with pituitary macroadenoma.
Another successful management case involved a cat with hyperadrenocorticism and a pituitary tumor. The treatment plan included radiation therapy using a linear accelerator delivering 4 Gy per fraction over 12 fractions. Gradual shrinkage of the pituitary gland was observed during CT and MRI examinations, indicating a positive response to treatment. This case study provided detailed insights into the treatment protocol of radiation therapy and the changes in clinical signs and radiographic findings in feline hyperadrenocorticism with pituitary macroadenoma.
These successful management cases demonstrate the potential effectiveness of radiation therapy in reducing pituitary tumor size and improving clinical signs in cats with hyperadrenocorticism. However, it’s important to note that individual responses to treatment may vary, and a comprehensive evaluation by a veterinarian is essential in determining the most suitable treatment approach.
Latest Research Findings
In a study involving 11 cats with pituitary tumors treated with radiation therapy, the treatment protocols varied, with doses ranging from a single 15-Gy dose to multiple doses of 15-20 Gy. Some cats showed improvement in clinical signs, including the resolution of diabetes mellitus, while others experienced adverse effects or required euthanasia due to other diseases (NCBI). These findings underscore the importance of individualized treatment plans and close monitoring of cats undergoing radiation therapy for hyperadrenocorticism.
Ongoing research continues to advance our understanding of hyperadrenocorticism in cats and its management. Researchers are investigating various treatment approaches, including radiation therapy, to optimize outcomes and minimize potential adverse effects. Staying informed about the latest research findings can help veterinarians and cat owners make informed decisions regarding the most appropriate treatment options for cats with hyperadrenocorticism.
By studying successful management cases and staying updated on the latest research findings, veterinarians can improve their treatment strategies for hyperadrenocorticism in cats. Additionally, cat owners can gain insight into the potential options for managing this condition and consult with their veterinarians regarding the best course of action for their furry companions.